Tibial Interlocking Nail Tips for Effective Recovery and Healing?
The Tibial Interlocking Nail has emerged as a pivotal tool in orthopedics, particularly for fracture stabilization. According to recent studies, this device significantly improves recovery times. For instance, data shows that patients treated with the Tibial Interlocking Nail experience a 30% faster time to full weight-bearing. The technique has gained traction among surgeons due to its effectiveness in reducing malunion rates.
Despite its advantages, some challenges remain. Not all patients respond uniformly to the Tibial Interlocking Nail. Factors such as age, overall health, and adherence to rehabilitation protocols can affect outcomes. Complications, while infrequent, can occur. They demand careful monitoring and sometimes additional interventions.
The importance of this device cannot be understated. Effective healing is crucial in restoring mobility and function. In certain cases, reflecting on the use of the Tibial Interlocking Nail reveals areas for improvement in surgical techniques and patient care protocols. This ongoing dialogue within the medical community is essential for maximizing benefits for all patients.
Tibial Interlocking Nails: Overview and Purpose in Bone Healing
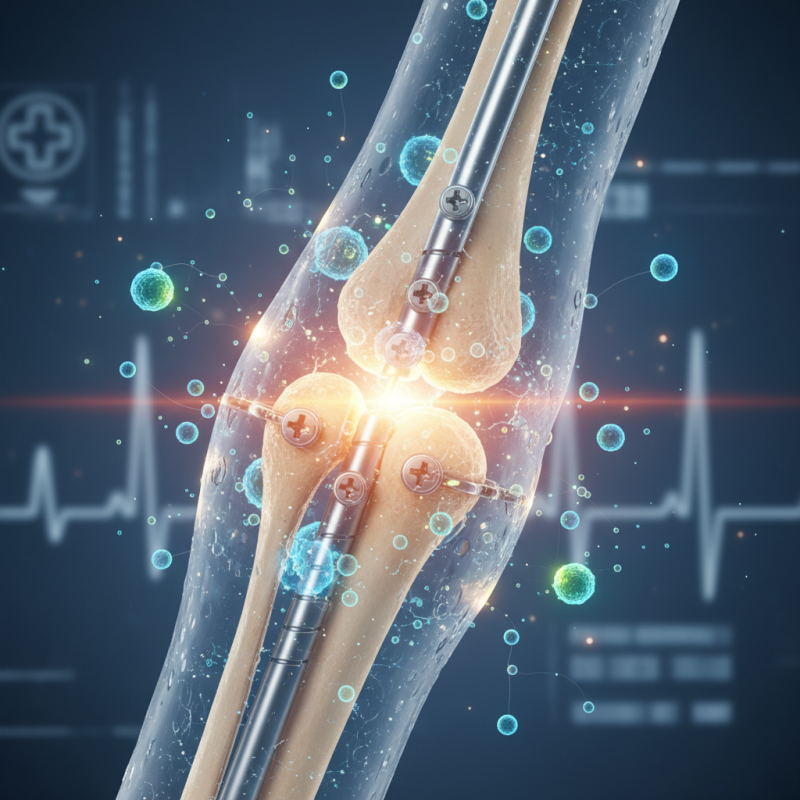
Tibial interlocking nails play a crucial role in the healing of bone fractures. These devices are inserted into the tibia to provide stability. They are often used in complex scenarios, such as when fractures occur in multiple places. The interlocking mechanism helps to secure the nails and prevents movement, which is vital for recovery.
Patients may experience discomfort or limited mobility post-surgery. Rehabilitation is a key part of the healing process. Physical therapy can help strengthen the muscles around the tibia. Importantly, the timeframe for recovery may vary. Some may heal within weeks, while others might take longer. Complications, though rare, can arise. Monitoring for infection or improper alignment is essential for effective healing.
Understanding the purpose of tibial interlocking nails can offer insights into bone healing principles. They are not a one-size-fits-all solution. Each case presents unique challenges. The journey to recovery is often non-linear, involving setbacks and progress. It's essential for patients to stay informed and engaged in their healing process.
Understanding the Anatomy of the Tibia and Its Healing Process
The tibia, commonly known as the shinbone, plays a crucial role in supporting the body's weight. It connects the knee to the ankle, providing stability and strength. When fractured, its healing process can be complex. The body initiates a cascade of biological responses, starting with inflammation, followed by the formation of a callus. This timeline can vary for each individual, often influenced by age and overall health.
Understanding the anatomy of the tibia is vital for promoting effective recovery. It consists of cortical and cancellous bone, which undergoes remodeling during the healing process. Proper alignment is essential; misalignment can lead to complications. This is where surgical interventions, like interlocking nails, come into play. They provide the support needed to keep the bone aligned during recovery.
Even with surgical aid, healing is not always straightforward. Some patients may experience slower recovery due to factors like pre-existing conditions or lifestyle choices. Regular monitoring and adjustments can be necessary. Patience is required, as the body may not always follow expected timelines. Each case should be assessed individually, allowing for flexibility and a tailored approach to recovery.
Mechanism of Action: How Interlocking Nails Promote Recovery
Interlocking nails have become a popular solution for tibial fractures. They provide stability and encourage proper alignment during the healing process. Understanding how these devices work can help patients grasp their importance in recovery.
The mechanism behind interlocking nails is fascinating. They work by providing mechanical support to the bone. When implanted, they stabilize the fracture site, allowing for early mobilization. This early movement can play a crucial role in recovery. Patients often report a quicker return to daily activities than with traditional methods. However, it's important to recognize that not all cases will have the same outcomes.
In some instances, complications may arise. Infection can occur around the surgical site, hindering the healing process. Additionally, some individuals may experience pain or discomfort from the nail itself. These challenges often lead to a need for further evaluation. Recovery isn’t always straightforward. It’s critical for patients to communicate openly with their medical team about their experiences during this process.
Post-Surgery Care and Rehabilitation Strategies for Patients
Post-surgery care is crucial for effective recovery when using a tibial interlocking nail. Patients often experience discomfort and immobility. It's essential to follow the surgeon's guidelines closely. Pain management is vital. Be proactive about reporting any unusual pain or swelling. Sometimes, medications can lead to side effects, requiring adjustments. Patients should communicate openly with their healthcare team.
Rehabilitation exercises play a key role in healing. Gentle movements can begin as soon as your doctor permits. However, progress may vary significantly from one person to another. Be patient, as some days will feel better than others. Consistency is important, even when frustration sets in. Setting small, achievable goals keeps motivation high.
Nutrition should not be overlooked. A balanced diet supports healing. Focus on proteins, vitamins, and minerals. Still, some patients may struggle with appetite. It’s normal to feel low sometimes. Seeking mental health support is just as important as physical recovery. Engage with support groups if feelings of isolation arise. Each step, no matter how small, is a step forward.
Potential Complications and Risk Factors Associated with Use
Tibial interlocking nails are commonly used for stabilizing fractures in the tibia. Though effective, potential complications can arise. According to a study published in the Journal of Orthopedic Trauma, infection rates following nail insertion can be as high as 6%. Additionally, delayed union or non-union of the fracture can occur in about 10% of cases, raising concerns about long-term recovery.
Patients may experience pain in the knee or ankle after surgery. This is often due to hardware irritation or misalignment. Research indicates that approximately 15% of patients report significant discomfort which may need further intervention. Some cases of malunion have been noted, leading to functional limitations. Patients must be informed of these risks before opting for surgical solutions.
Another consideration is the potential for complications related to the surgical procedure itself. Nerve or vascular injuries can happen, with reported incidences around 2-3%. There is also a risk of deep vein thrombosis, particularly in immobilized patients. Overall, while tibial interlocking nails provide stabilization, awareness of these complications is essential for patient safety and effective recovery.
Tibial Interlocking Nail Tips for Effective Recovery and Healing
| Parameter | Details |
|---|---|
| Procedure Success Rate | 85% - 95% |
| Average Recovery Time | 3 - 6 months |
| Common Complications | Infection, non-union, hardware failure |
| Risk Factors | Smoking, diabetes, obesity |
| Post-operative Care Recommendations | Physical therapy, weight management, smoking cessation |
| Follow-up Schedule | Every 4 - 6 weeks until healing is confirmed |
